In Oedipus Rex, a blind prophet named Tiresias tells Oedipus that he is the murderer he seeks and predicts that he will become a blind wanderer who was exiled from his own kingdom, all of which proves true to Oedipus’ dismay. Although I am no Tiresias with the ability to prognosticate with certainty, I tend to agree with experts who insist that we will likely not see something quite like this pandemic again in our lifetimes. However, we all may witness another emerging infectious disease, such as the coronavirus culprit — referred to in the scientific literature as SARS-CoV-2 — behind COVID-19, or a reemerging infectious disease like tuberculosis. Given our limited understanding of the multiple viral strains leading to COVID-19, it is crucial that we, as members of a global community sharing an exigent concern be able to process the deluge of information we are receiving from various sources. Whether you are hearing about the new cases reported in your local area on the news or reading about the acceleration of the COVID-19 pandemic worldwide, there is an underlying logic to contextualize and make sense of the numbers. This underlying logic has a name: transmission dynamics.
In infectious disease epidemiology and other disciplines, transmission dynamics involves capturing different information about the number of a.) healthy individuals, b.) currently infected individuals and c.) previously infected individuals to determine how each group changes and interacts over time. The application of this concept to outbreaks of any scale typically involves complex statistical modeling based on available data. While it is easy to get lost in the weeds with many modeling techniques, there is a common thread embedded in almost all of these transmission dynamics models called the “SEIR” model, which stands for susceptible (S), exposed (E), infected (I), and removed (R). Based on the work of Kermack and McKendrick from 1927, the SEIR model is a compartmentalized look at what is happening in a population at risk of a particular disease.
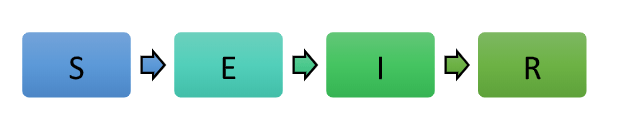
Given the relative simplicity of this model, it is not hard to see why this is a starting point for more intricate models attempting to estimate past, present, and future rates of infection and downstream consequences. Although this model is more parsimonious than most, it does make several critical assumptions, which adds a dimension of complexity to it. Due to the model’s assumptions, each letter of the SEIR acronym represents a compartment that has exclusive “membership” requirements. What this means is that members of a population can only be in one compartment at a time. In addition to this exclusivity requirement, the SEIR model is a deterministic model, which means that it generally assumes no randomness (also known as stochasticity in epidemiological research) in movement (represented by the arrows) from one compartment to another.
While the SEIR model is useful in developing our initial understanding of something like the COVID-19 pandemic, it may not be sufficient to predict the pathogen’s future spread and other patterns like infectivity and virulence accurately. Recently, there has been discussion about how “social distancing” and other widespread public health measures can lead to “flattening the curve.” What this “flattening” means is controlling the incidence density rate or the number of new cases of SARS-CoV-2 infection during a given time period. In the context of the SEIR model, social distancing affects how many “S” or susceptible individuals move to the “E” or exposed compartment. Washing our hands is the most convenient way to prevent moving from exposure to infection, but avoiding exposure in the first place is the most effective way to prevent infection. While we cannot wholly control migration from the “E” or exposed to the “I” or infected compartment, we can slow down the number of susceptible people exposed to SARS-CoV-2 to give the infected group a chance to move to the “R” or removed compartment. This is particularly significant given the finite availability of our healthcare resources across the world.
One other limitation of this simplistic model is that, in reality, not every member in each compartment has the same probability of moving through the sequence at the same rate or to the same outcome. The rationale for the stringent protective measures in place in the United States and other countries comes down to keeping as many people in the “S” compartment for as long as possible. The media has repeatedly emphasized how the elderly and older adults with multiple medical issues are particularly susceptible to severe, potentially fatal complications of COVID-19. Unfortunately, we must remember that the “R” in the SEIR model means “removed,” which indicates a person has recovered from the infection or has died. Given what we are beginning to understand about carrier states and undetectable infections related to SARS-CoV-2, we can revise the SEIR model to reflect more of what might be going on with the transmission dynamics.
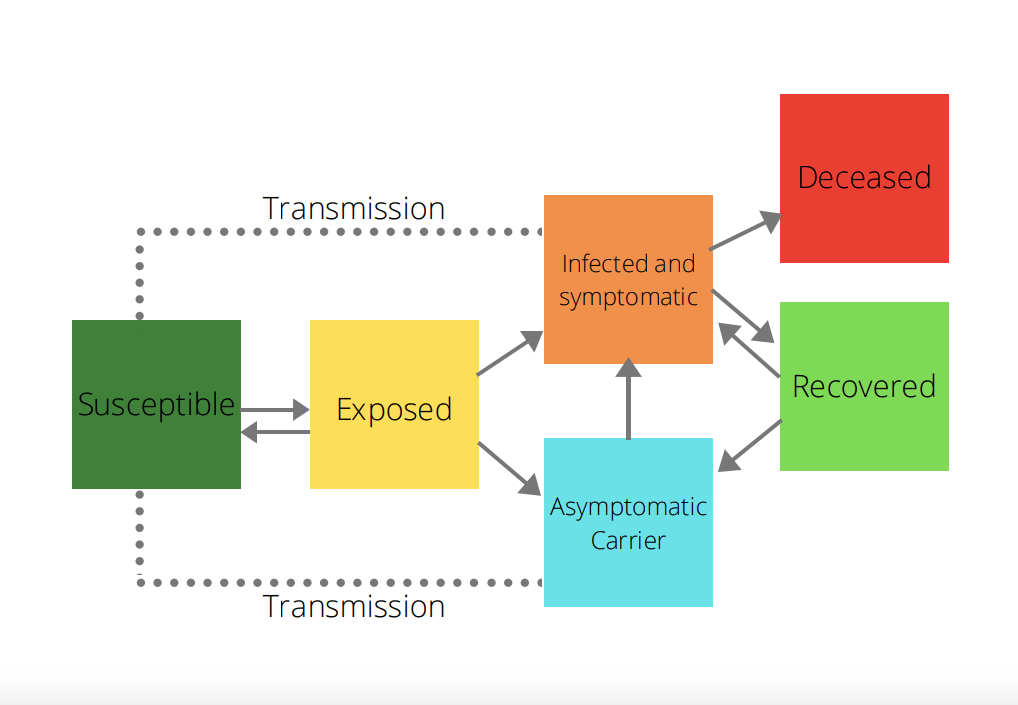
As our understanding of the pandemic increases, so too will our transmission dynamics models. Despite how complex the modeling becomes, they fundamentally rely on SEIR modeling principles and assumptions. Scientific knowledge is not static; it is as dynamic as a pathogen causing disease in a population. I encourage everyone to be open-minded about changing information because our models are only as strong as the data available at the time they are created or modified. The primary mechanism by which we obtain the most useful and timely data is disease surveillance systems, which have been challenging to strengthen due to underfunding limiting more resource-intensive yet more accurate types of surveillance strategies. What we can learn from this pandemic is that our public health infrastructure is not only valuable for keeping us safe during outbreaks of infectious diseases but also for understanding what is happening in our population earlier.
I urge my fellow community members to be critical of the information they are receiving and to use these basic principles to wade through the waters of COVID-19. During this pandemic, we should approach what the media are presenting with skepticism and an evidence-informed perspective that understanding the epidemiological theory of transmission dynamics enables. This insight allows all of us concerned with the rampant politicization and misinformation associated with the virus to make a positive impact on our communities. Eventually, we will see the end of this pandemic. We should use this experience as an opportunity for growth and re-assessment of our priorities as a national and global community, which starts with looking at how we can make our public health infrastructure a continually top priority for improving the country’s health.




Pingback: Intervene Upstream Issue 3 - Underlying: Reflections on Condition » Intervene Upstream, the online peer-reviewed public health publication for graduate students