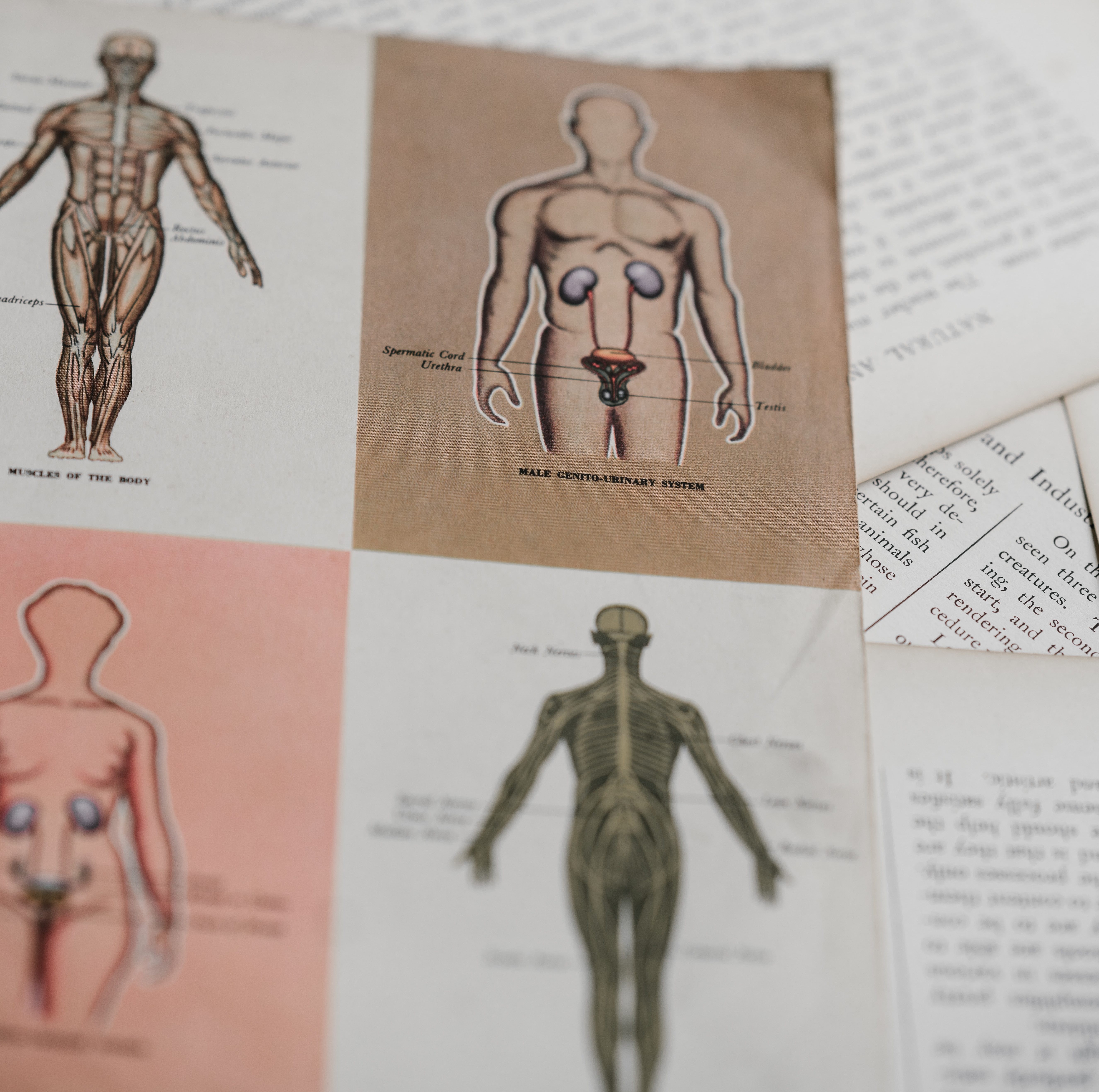
Herpes, syphilis, HPV, chlamydia, gonorrhea: don’t be mistaken, this is not the sexually transmitted infection (STI) version of the oh-so-popular Pepto Bismol commercial. No, this is just a short list of STIs students in many high school health classes are shown photos of as a scare tactic in an attempt to prevent them from having pre-marital sex. Although teen pregnancy rates have been on the decline since the early 90s, falling from 117 per 1,000 to 57 per 1,000 in 2010, the U.S. still has the highest teen pregnancy rate in the developed world, and in 2018, teens accounted for around half of newly diagnosed STIs. It is no wonder that the US is still combating this issue: less than half of U.S. states require sexuality education to be age-appropriate, and only 33 states require the sexuality education curricula to be medically accurate. Inaccuracies in these programs range from citing STIs as a consequence of premarital sex to withholding anatomically correct pictures and diagrams for being “oversexualized and detrimental to young men and women’s minds.” Without comprehensive sexuality education (CSE) that is age-appropriate, medically accurate, and evidence-based, how can we be sure our youth are adequately informed and protected before engaging in sexual activity? By implementing CSE nationwide, we can be sure youth are more aware and accurately informed of important reproductive health topics that most abstinence-based models fail to address.
Comprehensive sexuality education: Why haven’t we done this already?
While the issue has been debated by many local officials, parents, teachers, and even students themselves, the largest opportunities – and obstacles – in adoption of CSE are at the federal level. Sexuality education is highly politicized. Longstanding disagreement between our two political parties has alternately directed federal funding into or away from CSE programs and has had a profound effect on the trajectory of states’ curriculums. Ongoing debates as to what exactly students should be taught regarding their sexual and reproductive health have resulted in incomplete and inadequate coverage of topics that can improve safer sex practices among teenagers. Among other things, the CDC School Health Profiles track sexuality education in our nation’s schools, including the percentage of schools in which teachers taught students how to access valid and reliable health information, products, and services related to HIV, other STDs, and pregnancy. This number ranged from 28.4% to 90.6% across the states. From the same report, the percentage of schools in which teachers taught all sexual health topics specific to pregnancy, HIV, and STIs in a required course for students in any of grades 9, 10, 11, or 12 was a disconcerting 3.9% to 86.8% (median of 42.8%) across the 50 states.
Yet, as debates over CSE continue, so too do adolescents continue to engage in sexual activities: “[95%] of Americans have sex before marriage and, on average, adolescents in the United States have sex for the first time at about age 17.”
Critics of CSE are opposed to its implementation as they are often misinformed about the content of the program. They voice concerns that exposing youth to sexuality through accurate, age-appropriate education will lead to an earlier initiation of sexual activity and increased number of sexual partners. However, studies have proven otherwise. CSE is defined as robust K-12 programs that cover a myriad of topics such as human development, relationships, personal skills, sexual behavior, sexual health, and society and culture. In fact, these programs have astounding results: a 2007 study of 56 curriculum-based programs showed that 63% had a significant positive impact on one or more types of sexual behavior, including decreasing number of sexual partners, delaying the initiation of sex, and increasing the uptake of condoms and other contraceptive methods.
Although implementing CSE curriculums cannot fully rectify all of the sexual and reproductive health issues our youth face, it is a sure step in the right direction in helping teens become better informed. Students are individuals and each come with a unique set of questions and concerns. It is therefore imperative to tailor approaches based on knowledge of those concerns and needs.
To our federal lawmakers:
Please think twice before banning CSE programs and funneling money to abstinence-based curriculums, which time and time again have been proven both ineffective and undesirable to many parents and health professionals. Consider your own children: would you want them to receive their sexuality information from a credible source?
State leaders:
Please advocate for your state’s adoption of CSE.
Dear teachers:
Embrace whatever curriculum is currently available to you, and please seek information about issues that students at your schools face. If possible, modify the curriculum and provide students with science-based knowledge and skills to make healthy and informed decisions. If this is not something you feel comfortable doing, please contact your school district and discuss inviting a licensed professional to administer the sexuality education lesson(s).
Finally, to parents:
Do not shy away from having conversations with your children. Creating a safe space for kids to talk about their concerns leaves less room for risky individual experimentation.
We reach for Pepto Bismol during periods of abdominal discomfort – it’s a safe, proven choice. What information will our kids reach for when they miss out on a comprehensive sexuality education experience in a safe academic setting? What sort of media and misinformation will they consume instead in search of answers to their questions? Most importantly, what long-term consequences will our children be faced with as a result of our attemps to shield them, in the short term, from important sexual health information that can equip them for a safer and healthier sex life in the future? Health is a human right, and adolescents deserve comprehensive sexuality education to stay safe and informed.